What Are the Symptoms of Dermatitis?
The main symptom of dermatitis, or skin inflammation, is dry, red, itchy skin.
There are many types of dermatitis. Symptoms can vary depending on the type of dermatitis you have.
Contact dermatitis
Contact dermatitis, caused by exposure to an irritant or allergic reaction, typically shows up as a red, itchy rash that is limited to the area of skin exposed to the substance.
Nummular dermatitis
Nummular dermatitis, common in people who have dry skin or live in dry environments, shows up as red, itchy, circular patches of weeping, scaly, or crusted skin.
Seborrheic dermatitis
Seborrheic dermatitis, called cradle cap in infants, causes greasy, yellowish scales on the scalp and eyebrows, behind the ears, and around the nose.
Stasis dermatitis
Stasis dermatitis causes scaling, darkening and swelling of the lower legs. Sometimes ulcerated or open skin appears inside the lower legs and around the ankles.
Atopic dermatitis (eczema)
Atopic dermatitis (eczema) can cause extreme, persistent skin itchiness. However, many times, itchiness results simply from dry skin.
Contact our dermatology office about dermatitis if:
- Your skin has oozing sores; honey-yellow crusting; red, swollen, tender areas; or other signs of infection. You may need treatment with antibiotics or other drugs.
- The affected skin does not respond to treatment with over-the-counter creams or medicated shampoos. You should have a medical diagnosis and treatment.
- You are exposed to anyone with herpes simplex virus infection while you are having a flare-up of atopic dermatitis (eczema). You are at increased risk of contracting the viral disorder.
Recognizing the symptoms of dermatitis is crucial for prompt and effective management. Whether it’s the red, itchy rash of contact dermatitis, the circular patches of nummular dermatitis, the greasy scales of seborrheic dermatitis, or the lower leg issues associated with stasis dermatitis, understanding the signs allows for targeted intervention. Particularly in cases of atopic dermatitis (eczema), where persistent itchiness may indicate more than just dry skin, seeking professional help from our dermatologist is imperative. If you observe oozing sores, crusting, swelling, or signs of infection, or if over-the-counter remedies prove ineffective, don’t hesitate to contact our dermatology office. Timely intervention can make all the difference in managing and alleviating dermatitis symptoms effectively. Your skin’s health is our priority.

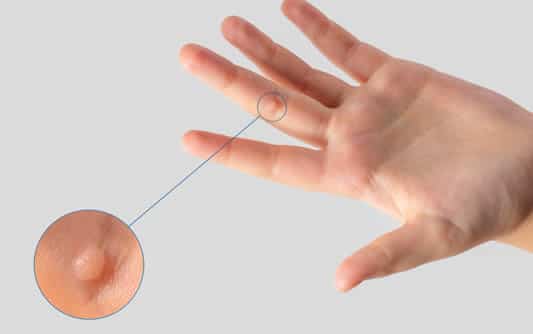
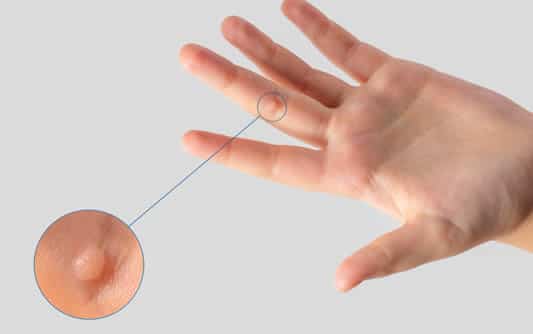
What Are Skin Tags?
Skin tags are often of no concern and do not require treatment or removal.
Many people, however, experience discomfort as skin tags can get snagged on clothing and jewelry. Others simply want to remove them for cosmetic reasons, which are equally valid.
Skin tags are soft, small flaps of tissue that protrude from the skin by a connecting stalk. They commonly form on the folds of skin in the neck, groin, armpits, and eyelids. These growths are loose collagen fibers that become lodged inside thicker areas of the skin. The cause of skin tags is unknown, but they pose no threat of developing into cancer.
4 Reasons Why You Should Seek Professional Care For Skin Tag Removal
Prevent Risk Of Infection
Professional medical experts have the proper sanitizing equipment and follow strict guidelines to ensure that there is no risk for infection when cutting into the skin. Removing skin tags at home often do not allow you to benefit from the same postoperative care as at a dermatologist. As a result, at-home removals can delay the healing site process and lead to scarring—or worse, a trip to the emergency room.
Prevent Loss Of Movement From Scarring
If a skin tag is removed incorrectly, scarring will result. If the scar is located on a joint, such as a knuckle or elbow, the scar will limit the mobility of that body part. Dermatologists use proper techniques to prevent excessive scarring, ensuring you retain full mobility in the joint.
Ensure The Entire Removal Of The Mole or Skin Tag
The risk of only removing the surface or part of a skin tag at home is high. You could be leaving most of the remaining portions deep within the skin layers. This can result in the regrowth of the skin tag and cause difficulties for medical professionals to remove it in the future.
Avoid Blood Loss
Skin tags can root deep inside your skin layers and may require an incision for correct removal. If you perform the incision without a medical professional, you will risk cutting the skin too deep or nicking a vein or blood vessel. This will cause uncontrolled bleeding and a trip to the emergency room.
While skin tags are generally harmless, seeking professional care for their removal offers several crucial advantages. From preventing infections and minimizing scarring to ensuring complete removal and avoiding potential blood loss, entrusting the process to skilled dermatologists ensures a safe and effective outcome. Whether motivated by cosmetic concerns or discomfort, choosing professional care provides peace of mind and preserves the integrity of your skin. Remember, your skin deserves the best care possible, so why not let the experts handle it?

Dry skin comes with aging. By 60 years of age nearly everyone has dry skin. If you also take certain medication, undergo cancer treatment, or receive dialysis, you can develop excessively dry skin.
What causes excessively dry skin?
When skin loses water too quickly, it becomes dry. This can happen for many reasons.
- Everyday things, such as using deodorant soaps and harsh cleaning products, can strip oils and fats from our skin.
- Taking long, hot showers can also dry your skin.
- Living in a cold, dry place dries the skin, too.
You can often heal dry skin by making some changes, which includes moisturizing several times a day.
When the skin continues to lose water and cannot heal itself, skin can become excessively dry. Age, certain medications, and disease can also cause skin to become excessively dry.
Who develops excessively dry skin?
Certain people have a higher risk of developing excessively dry skin. If any of the following apply to you, you may. How many of the following apply?
- Middle age or older: With age, our skin produces less sebum, an oil that keeps skin soft and youthful. By your 40s, the amount of sebum your body makes drops dramatically. After 40, the amount of sebum your skin contains continues to drop.
- Black, brown, or fair skin: Research shows that people who have brown, black, or fair skin are more likely to develop very dry skin than people who have a medium complexion, such as people who have Mediterranean ancestry.
- Certain medications: Extremely dry skin is a possible side effect of several medications, including statins and diuretics.
- Wet work: A job that requires you to frequently put your hands in water throughout the day or use harsh chemicals can strip your skin of its protective layer. Hairdressers, nurses, housekeepers, construction workers, cooks, florists, and metal workers often develop excessively dry skin.
- Low outdoor temperature: When outdoor temperatures fall, the air holds less moisture. Research shows that this can lead to excessively dry skin.
- Vitamin or mineral deficiency: Skin requires nutrients to keep it healthy. If you’re not getting enough vitamin D, vitamin A, niacin, zinc, or iron, you can develop excessively dry skin.
- Smoking: Cigarettes contain harmful chemicals that speed up how quickly your skin ages, so skin becomes drier.
- Condition that affects the skin: Some conditions that affect the skin, including atopic dermatitis, ichthyosis, perioral dermatitis, psoriasis, and seborrheic dermatitis, can cause excessively dry skin.
- Itchy skin condition: If you’ve had a skin condition that caused itchiness at some time in your life, you have a greater risk of developing excessively dry skin. Many adults who had atopic dermatitis as a child live with extremely dry skin.
- Diabetes, thyroid disease, or kidney disease: These conditions are known to cause excessively dry skin.
- Dialysis: Kidney disease increases your risk of developing extremely dry skin. When you receive dialysis, you have an even greater risk because dialysis removes water from your body. People receiving dialysis treatments also need to limit how much fluid they drink, consuming only 32 ounces a day. This can further dry your skin.
- Cancer treatment (current and past): If you’ve ever had chemotherapy, are receiving a cancer treatment called targeted therapy, or getting radiation treatments, you can develop extremely dry skin.
- Anorexia: If you’re not eating enough, you’re not getting the nutrients your skin needs to stay hydrated.
- HIV positive: Excessively dry skin is common in people who are HIV positive, even those on antiretroviral treatment (ART).
If you develop excessively dry skin, dermatologists recommend treating it. Treatment can prevent the condition from worsening.
Should the dry skin worsen, you can develop permanent side effects. Your skin can itch most of the time. Some people develop food allergies. It’s also possible to develop irritated skin every time you touch certain objects. You also have a higher risk of developing a serious skin infection.

If you are one of the millions of men who suffer from male pattern baldness, you know that it can be a frustrating and embarrassing condition. While it is not always possible to predict and prevent male pattern hair loss, there are treatments that can slow the progression of hair loss and even help you regrow a fuller head of hair.
Causes of Male Pattern Hair Loss
Male pattern baldness, or male pattern hair loss, is the most common type of hair loss in men. Formally known as androgenetic alopecia, this condition is characterized by a receding hairline and thinning of the hair on the top and sides of the head. Male pattern baldness is usually caused by a combination of genes inherited from one or both parents. Each affected male’s unique genetic combination predicts age of onset, pattern, progression, and severity of hair loss. Male sex hormones (androgens) also play a role in the development of androgenetic alopecia.
Male pattern hair loss is very difficult to predict, and once it begins, the hair loss will continue. The hair will become increasingly fine, and the hair follicles will gradually diminish over time. Eventually, there will be bald spots where no hair grows at all (hence the common name “male pattern baldness”).
Effective Treatments for Male Pattern Baldness
The vast majority of men over age 50 have some extent of male pattern hair loss. Despite the prevalence of this condition, many affected men (especially those with premature or accelerated hair loss) experience anxiety and a negative impact on their self-esteem as a result. If you fall into this category, don’t worry — there are effective hair loss treatments available to you. The following treatments offered here at Kirsch Dermatology may help slow down your hair loss and, in many cases, even regrow your hair.
- Minoxidil (Topical and Oral): This medication can help individuals with androgenetic alopecia regrow hair.
- Oral Finasteride and Dutasteride: These medications can slow hair loss in the middle and crown of the head, promote new hair growth, and prevent further hair loss.
- Ketoconazole Prescription Shampoo: This antifungal shampoo can prevent hair follicle shrinkage and minimize hair loss.
- HydraFacial Keravive™: This in-office dermatology treatment nourishes hair follicles to promote a healthy scalp with fuller hair.
- HydraFacial Keravive™ Peptide Complex Spray: Daily use of this spray in combination with in-office HydraFacial Keravive™ treatments promotes healthy hair follicles for fuller, healthier hair.
- PRP (Platelet-Rich Plasma): Growth factors found in platelet-rich-plasma (extracted from your own blood) can stimulate hair regrowth and may be especially beneficial for those with early hair loss.
- Vitamin and Nutritional Supplementation: Where appropriate, certain vitamin and nutritional supplements may assist in the prevention and treatment of male pattern hair loss.
Contact our dermatology office to see what options we offer for hair loss treatment in Bakersfield

Regularly checking your skin can help catch skin cancer early, when it’s highly treatable. Follow these tips from board-certified dermatologists to check your skin for signs of skin cancer.
Anyone can get skin cancer, regardless of skin color, age, or gender. It is estimated that one in five Americans will develop skin cancer in their lifetime. When caught early, skin cancer is highly treatable.
You can detect skin cancer early by following dermatologists’ tips for checking your skin. Download the AAD’s body mole map to document your self-examination, or the How to SPOT Skin Cancer™ infographic and know what to look for when checking your spots.
If you notice a spot that is different from others, or that changes, itches or bleeds, partner with the skin cancer expert, a board-certified dermatologist.
How to perform a skin self-exam
- Examine your body in a full-length mirror
- Examine your body front and back in a full-length mirror, then look at the right and left sides with your arms raised.
- Look at your underarms, forearms, and palms
- Bend your elbows and look carefully at your forearms, underarms, fingernails, and palms.
- Look at your legs, between toes, and soles of your feet
- Look at the backs of your legs and feet, the spaces between your toes, your toenails, and the soles of your feet.
- Use a hand mirror to examine your neck and scalp
- Examine the back of your neck and scalp with a hand mirror. Part your hair for a closer look at your scalp.
- Use a hand mirror to check your back and buttocks
- Finally, check your back and buttocks with a hand mirror.

One easy way to remember common characteristics of melanoma is to think alphabetically – the ABCDEs of melanoma. ABCDE stands for:
- Asymmetry
- Border
- Color
- Diameter
- Evolution
These are the characteristics of skin damage that doctors look for when diagnosing and classifying melanomas.
Asymmetry
Melanoma is often asymmetrical, which means the shape isn’t uniform. Non-cancerous moles are typically uniform and symmetrical in shape.
Border
Melanoma often has borders that aren’t well defined or are irregular in shape, whereas non-cancerous moles usually have smooth, well-defined borders.
Color
Melanoma lesions are often more than one color or shade. Moles that are benign are typically one color.
Diameter
Melanoma growths are normally larger than 6mm in diameter, which is about the diameter of a standard pencil.
Evolution
Melanoma will often change characteristics, such as size, shape or color. Unlike most benign moles, melanoma tends to change over time. If you have a mole or skin growth, watch it for signs of changes. If you notice any of the ABCDEs of melanoma, make an appointment right away to be evaluated by a dermatologist.
We recommend doing regular skin checks at home to look for changes in your skin. Call it an ABCDE assessment. If you notice any of the signs and symptoms of melanoma or you have a suspicious mole or lesion, make an appointment to see your doctor. You may want to have annual skin checks with a dermatologist as well so you can catch skin cancer before it becomes life threatening.
Skin cancer is common, and when it’s caught early, most skin cancer – including melanoma – can be cured.
If you see something on your skin, don’t panic. Most skin lesions and moles are not cancerous, but it’s always best to get checked out to be sure.

If you have dark spots on your skin, it can be hard to tell if it’s hyperpigmentation or melasma, as both are extremely common. While they are two different dermatological conditions, they can look and act alike, and they are both caused by similar things. Here, the expert dermatologists at Columbia Skin Clinic take a closer look at the similarities and differences of hyperpigmentation vs. melasma to help you distinguish the two.
Hyperpigmentation
Hyperpigmentation is an umbrella term used to cover any number of conditions where one patch of skin becomes noticeably darker than the surrounding skin of the same area. This term covers a number of more specific conditions such as liver spots, freckles, and melasma.
Although different types of hyperpigmentation can be caused by various factors such as acne scarring, medications, or inflammation from other conditions, the main cause of hyperpigmentation is sun exposure. When we leave our skin untreated, harmful UV rays from the sun cause damage. This damage manifests itself in many ways, from harmless freckles to more severe conditions like skin cancer. Many of these conditions fall under the category of hyperpigmentation.
Most hyperpigmentations are harmless, and many forms are readily treatable through a mixture of options such as topical creams, Vitamin C, and cosmetic treatments. With most examples of hyperpigmentation, the patient only needs to be concerned with physical appearance and does not need to worry about more serious, long-lasting health effects. However, it’s always important to get any area checked out by a dermatologist just to make sure.
Melasma
One specific type of hyperpigmentation is melasma, a condition that affects over 5 million Americans. Although it also is a type of condition characterized by darker patches of skin, melasma is differentiated from other forms of hyperpigmentation mainly by its cause; rather than just being sun-related, melasma is caused in part by hormonal changes within the body. This is why melasma is often referred to as “the mask of pregnancy,” as pregnant women are much more likely to have this condition. In fact, melasma is found much more prevalently in women – pregnant or not – partly because of this hormonal cause.
Melasma is also referred to as a “mask” because it almost always targets a person’s face, resulting in dark patches of skin on a person’s chin, cheeks, nose, upper lip, or other cranial areas. Melasma can sometimes be found in other parts of the body, typically those prone to more sun exposure, such as the shoulders. While not dangerous, the location of these dark patches can lead to discomfort in public.
Melasma Treatment
In addition to its causes, another distinguishing feature of melasma is its difficulty in treatment. Whereas some types of hyperpigmentation can be treated with topical creams, melasma is not treated so easily due to the hormones that contribute to its cause in the first place.
Even though most treatment options are the same as other forms of hyperpigmentation, the success rate is typically much lower. Because hormones are a personalized set of chemicals, each person’s melasma responds differently to treatment, making it notoriously difficult to treat.
Most dermatologists recommend a combination of treatments, including strong sunblocks, vitamins, and brightening agents such as hydroquinone. To an extent, using a wide variety of treatments is less about creating a “shock and awe” approach as it is trying a variety of methods all at once in the hope that we can find the right treatment.
In some cases, the melasma can clear up quickly. In other cases, it might take a while longer. For some people, treatments must be repeated indefinitely, or the melasma returns. Just as each individual’s hormones are different, each person’s response to treatment is different, making it almost impossible to predict who will respond well and who will take more time and effort.
The Importance of Sun Protection
The most significant commonality between hyperpigmentation in general or melasma specifically is sun exposure. The harmful effects of solar radiation are well-known today, and yet people still take risks by venturing outside without proper protection.
The various types of hyperpigmentation, including melasma, are all triggered in part by prolonged exposure to the sun. To make matters worse, it is impossible to know how much sun exposure is too much until it’s too late and the damage has already been done. The importance of wearing proper clothing and applying sunscreen cannot be overstated if you wish to avoid these unsightly conditions at some point in your future.

Eczema and Your Diet: What to Eat and What to Avoid to Minimize Flare-Ups
Eczema is an inflammatory skin disorder that results in red, dry itchy skin. Also called dermatitis, eczema can result in skin bleeding and crusting over in the folds of the arms, back of the knees, wrists, and hands. Eczema is a very personal condition in which each person has different triggers and responds well to different treatments.
Individuals who struggle with eczema can have flare-ups triggered by certain foods. Your diet can have a huge impact on the quantity and severity of eczema patches. Because it is an inflammatory condition, the best foods to eat are ones that counteract the inflammation. Additionally, most patients with eczema suffer from food allergies that can trigger flare-ups. It is important to know what foods work in your body to minimize the presence of eczema.
Eczema Diet Tips
Foods to Include for Eczema:
- Foods that contain anti-inflammatory properties include fish, probiotic foods, and foods high in quercetin. Fatty fish contain high levels of omega-3 fatty acids which is a crucial nutrient in fighting inflammation. Salmon, tuna, and sardines are all very high in omega-3s. You can also take an omega-3 supplement if fish does not appeal to you.
- Foods that contain probiotics (live cultures) build up a strong immune system in your gut and this helps reduce flare-ups. There are lots of options when it comes to foods that contain probiotics including sauerkraut, fermented pickles, sourdough bread, yogurt, kimchi, and miso soup.
- Quercetin is a flavonoid (chemical nutrient) found in plants. Quercetin specifically gives plants their rich color, is an antioxidant, and an antihistamine. The best foods to eat that contain quercetin are apples, blueberries, spinach, broccoli, cherries, kale, and onions. Eating a wide variety of the previously mentioned foods will help to control eczema symptoms.
Foods to Avoid for Eczema:
- Inflammatory foods can trigger an increase in symptoms. Added artificial sugars, trans-fats, processed meat, red meat, refined carbs, and dairy all cause inflammation in the body.
- Foods containing nickel. Nickel is an ingredient known to encourage symptoms of dyshidrotic eczema. Dyshidrotic eczema is a type of eczema that produces small blisters on the hands and the feet. Nickel is found in whole wheat and grains, rye, oats, cocoa, baking powder, soy products, canned foods, and dried fruits.
Allergies or Sensitivities
Your doctor may perform an allergy or food sensitivity test to see what foods your body cannot tolerate. After exposure to certain foods, your body might react in what is called “food responsive eczema.” If you do test positive for an allergy or sensitivity, it is crucial to avoid consuming those foods. Common food allergens are dairy, eggs, soy, and nuts.
Elimination Diet
If you are struggling with eczema flare-ups and are looking for ways to help your systems, you may want to try an elimination diet. This diet is done by removing foods or food groups that you suspect you may be intolerant to. When it comes to an elimination diet for eczema specifically, it is best to eliminate common allergens and inflammatory foods. Remove these foods from your diet for at least 3 days to see if symptoms subside. Try removing one food at a time so you know exactly what is contributing to your symptoms. By only removing one food at a time, this also allows you to have more freedom as you will not be limiting too much of your diet.
In conclusion, eczema is a condition that varies from person to person. Symptoms can be triggered by many different environmental and internal factors. When it comes to managing your symptoms through your diet, it is a process of trial and error. Finding the best foods to fight your eczema condition will take some time, but eventually, you will be able to determine what to eat and what to avoid for the best results. If you are struggling with eczema and cannot seem to find any relief, you should contact your dermatologist. They will create a treatment plan just for you to help treat this dermatology skin condition.

Living with Psoriasis is a unique challenge – one that can be both physically and emotionally trying. You may feel embarrassed when your symptoms flare up, confused about the best treatments to seek out, or overwhelmed by feelings of anxiety and sadness. But it’s important to remember that you are not alone in this battle, and there are resources available to help you cope with and manage your condition.
Coping Strategies for Managing Symptoms
Psoriasis is a skin condition that affects millions of people worldwide and can cause discomfort and embarrassment. Coping with the symptoms of Psoriasis can be a challenging experience but there are effective ways to manage it. With the right knowledge and treatment, people can reduce the severity and frequency of flare-ups as well as improve their quality of life. Here are a few strategies for coping with the symptoms:
Stress Control
Many individuals with Psoriasis have found that stress can exacerbate their symptoms. But here’s the good news – you can break this cycle. By learning how to effectively manage stress, you can not only alleviate flare-ups but also reduce overall inflammation in your body. Explore the power of meditation, exercise, or even seek guidance from a specialized stress management therapist.
Dietary Changes
Discover the power of a healthy diet in optimizing body function, diminishing comorbidity, and enhancing metabolic profile. Research into the connection between diet and Psoriasis is ongoing. Supplementing with vitamin D, especially in the winter months, may also help reduce flare-ups.
Lifestyle Changes
Those dealing with Psoriasis should avoid alcohol and smoking, which can trigger the body’s inflammatory response. Getting plenty of sleep and routine exercise can help you avoid flare-ups. When outside, use sunscreen to protect your skin from sunburn, which can also cause flare-ups.
Moisturize Your Skin
Keeping skin moisturized is also a key technique. Dryness can cause flare ups and result in skin scaling. Look for moisturizers that contain mineral oils like liquid paraffin and petrolatum. Coconut oil and aloe vera gel are also great options due to their anti-inflammatory and antibacterial properties.
Treatment Options for Controlling the Condition
There are quite a few treatment options available that can help manage the symptoms and alleviate some of the discomfort associated with Psoriasis. From topical creams and ointments to phototherapy and systemic treatments, there’s bound to be a solution that works for you. We’ll touch on just a few of them below.
Topical Treatments
Topical treatments, such as corticosteroids, vitamin D analogs, and retinoids, work by reducing inflammation and suppressing the immune response that causes Psoriasis. Some options include:
-
-
- Steroid creams
- Salicylic acid
- Calcipotriol
- Roflumilast
- Tapinarof
- Tazaroc
Phototherapy
Phototherapy has emerged as an effective and safe treatment option. This light therapy has been used to treat skin conditions for centuries, with modern advancements making it even more effective. Psoriasis patients have reported improvements in their symptoms after undergoing this treatment, which involves exposure to ultraviolet light.
Natural Treatments
From herbal remedies to dietary changes, there are a variety of ways to approach treating this complex skin condition without relying on traditional medications. While it’s important to consult with a dermatologist before making any major changes, many people have found success with natural remedies like aloe vera, turmeric, and coconut oil. Additionally, incorporating anti-inflammatory foods like leafy greens, berries, and fatty fish can help to reduce inflammation and improve overall skin health.
Other Treatments
These are just a few of the treatment options. Other treatments include immunosuppressants, oral retinoids, and systemic biologic treatments. Some treatments will work better for some and less so for others, so it may take some time to find the best treatment for your condition.
Relief Is in Sight
Despite the fact that Psoriasis is incurable, it’s important to remember that there is still hope for those who suffer from it. With the right treatment regimen and a bit of patience, you can learn to manage your symptoms and live a full and happy life.
Over-the-counter salicylic acid is a commonly used medication to treat your warts. The salicylic acid is slowly and painlessly absorbed into the skin causing peeling of the skin cells that contain the wart virus. This is a very good way of getting rid of warts, but it should never be used to treat warts on the face, neck, and genitals. Even if another treatment is being used (for example in-office freezing or beetle juice), using salicylic acid at home speeds destruction of the wart by thinning it and any callus that has formed on or around it.
Salicylic acid preparations can be found in most drugstores and some supermarkets. There are typically two kinds of products: adhesive pads that are treated with salicylic acid or bottles of concentrated salicylic acid.
Products available typically include:
- 17% Salicylic Acid Topical Liquid (Compound W or Dr. Scholl’s*)
- 40% Salicylic Acid Topical Liquid (Plantar Wart Remover*)
- 40% Salicylic Acid pads (Corn Removal Pads*)
- *Any store brand product with the recommended percent salicylic acid will work
Salicylic Acid Wart Treatment
Thin down the wart with a pumice stone or nail file. File the area until all the white, dead skin is removed without causing discomfort or pain. Make sure not to share pumice stones or nail files because the wart virus can be transmitted on these. Sometimes soaking the wart in warm water helps to soften the wart. You may soak the wart for 5-10 minutes before filing it down.
Apply the solution or pad(s) to the wart(s). You may cut pads to size if necessary.
Cover with a Band-aid or duct tape. If the wart is on a less workable area, such as the finger, smaller electrical tape may work better since it stretches.
Repeat process every night before bed until your next appointment.
Note:
Stop sooner if the wart falls off, swelling/drainage develops at the site, or the area becomes too irritated or painful. Please call the dermatology clinic if these symptoms persist.
This wart treatment should be well tolerated and easy to use at home. Some mild discomfort, burning, skin redness, and peeling is expected while using the wart treatment. This means that the wart is going away.